Abstract
Response to induction therapy is a powerful prognostic indicator in acute myeloid leukemia (AML). Measurable/minimal residual disease (MRD) assays are being increasingly incorporated into response assessment; however, their value as a surrogate for long-term outcome remains unclear because of assay limitations and the effect of post remission therapies. This is particularly the case for the molecularly heterogeneous NPM1 wild type standard risk patients for whom treatment decisions, including predicting the benefit of allogeneic stem cell transplantation (SCT), are particularly challenging. We investigated the effect on outcome of MRD status compared to other response criteria after each cycle of induction for NPM1 wild type (wt) standard risk patients and other risk groups in a cohort of younger AML patients.
Patients and Methods
As part of the UK NCRI AML17 trial (ISRCTN55675535) for patients with AML or high risk MDS up to the age of 60, prospective flow cytometric MRD (MFC-MRD) monitoring was performed after each course of induction. Any level of MRD detected was considered MRD+ (sensitivity thresholds: ~0.02% by tracking diagnostic leukemic aberrant phenotypes/LAIP, ~0.05-0.1% by "different-from normal" blast LAIP). Clinicians were not informed of MFC-MRD results. Following cycle 1 of induction with daunorubicin/ara-C based therapy, patients were allocated a risk group by a validated score (comprising cytogenetics, WBC, age, secondary disease, blast response to cycle 1 and mutation status). Standard risk patients including ITD wt/ NPM1 wt received a second daunorubicin/ara-C induction with some proceeding to SCT after 1 or 2 consolidation cycles (high dose ara-C).
Results
2450 non APML patients, median age 51, randomised 4/09 to 12/14, contributed data. For the total cohort, 5 year overall survival (OS) excluding early deaths was 52% for those achieving CR/CRi vs 31% for those not in CR (p<.001).
Post cycle 1 (C1) responses were categorised as resistant disease (RD), partial remission (PR) and CR/CRi by clinicians, with CR/CRi subdivided by MFC-MRD assay into MRD+ and MRD-. RD vs PR vs MRD+ vs MRD- frequencies were 15% vs 14% vs 40% vs 31% for all patients with response data (n=1443), 5% vs 7% vs 45% vs 43% for good / standard risk (n=785), 10% vs 8% vs 47% vs 35% NPM1 wt standard risk (n=320).
Post C1 response was prognostic for survival: OS for RD vs PR vs MRD+ vs MRD- were 25% vs 36% vs 43% vs 63% all patients; 33% vs 49% vs 51% vs 70% good/standard risk and 28% vs 38% vs 47% vs 59% NPM1 wt standard risk. (p<.0001 throughout). For NPM1 wt standard risk as well as good/standard risk patients adjusted analyses confirmed significant OS differences between C1 RD vs PR or MRD+ but not PR vs MRD+. Results were similar when censored at SCT.
Post C1 best response was CRi for 39/446 MRD- vs 49/575 MRD+ overall (11/111 vs 8/149 for NPM1 wt standard risk). C1 CRi was associated with reduced OS overall (39% vs 53% CR, p=.002) and in MRD+ (19% vs 45% CR, p=.001) but not for MRD- patients. OS for NPM1 wt standard risk MRD+ was 25% CRi vs 43% CR (p=0.4). No significant difference was detected for 5 year cumulative incidence of relapse (CIR).
The effect on outcomes of MRD status post cycle 2 (C2) for the 806 patients in CR/CRi with MFC-MRD data appeared greater (relapse HR 1.88(1.50- 2.36), p<0.001; OS HR 1.77(1.41-2.22) p<0.001)than C1 (relapse HR 1.70(1.40- 2.06), p<0.001; OS HR 1.50(1.23-1.84) p<0.001). MRD+ levels of ≥0.1% predicted highest CIR in NPM1 wt standard risk patients at C1 (CIR 71%) and C2 (CIR 89%) but any MRD+ at C2 reduced OS (32% vs 63% MRD-, p=0.003) and OS censored at any SCT (35% vs 88%). The effect of CR vs CRi was smaller post C2 although outcomes were still worst in CRi/MRD+ve patients.
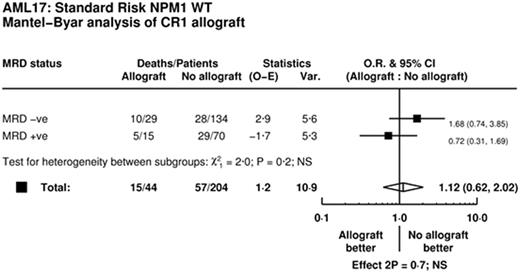
Of 204 NPM1 wt standard risk patients with C2 MRD data 83 had an allograft (44 in CR1: 29 MRD-, 15 MRD+). In Mantel-Byar analyses, although numbers were small, there was a suggestion that transplant could be considered in MRD +ve (HR 0.72 (0.31-1.69)) but not MRD -ve patients (HR 1.68 (0.75-3.85); p-value for interaction p=0.16).
Conclusion
MRD status by MFC refines response criteria at induction time-points to differentiate NPM1 wild type standard risk patients with poor outcome and helps define a group of patients who may benefit from SCT in CR1.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal